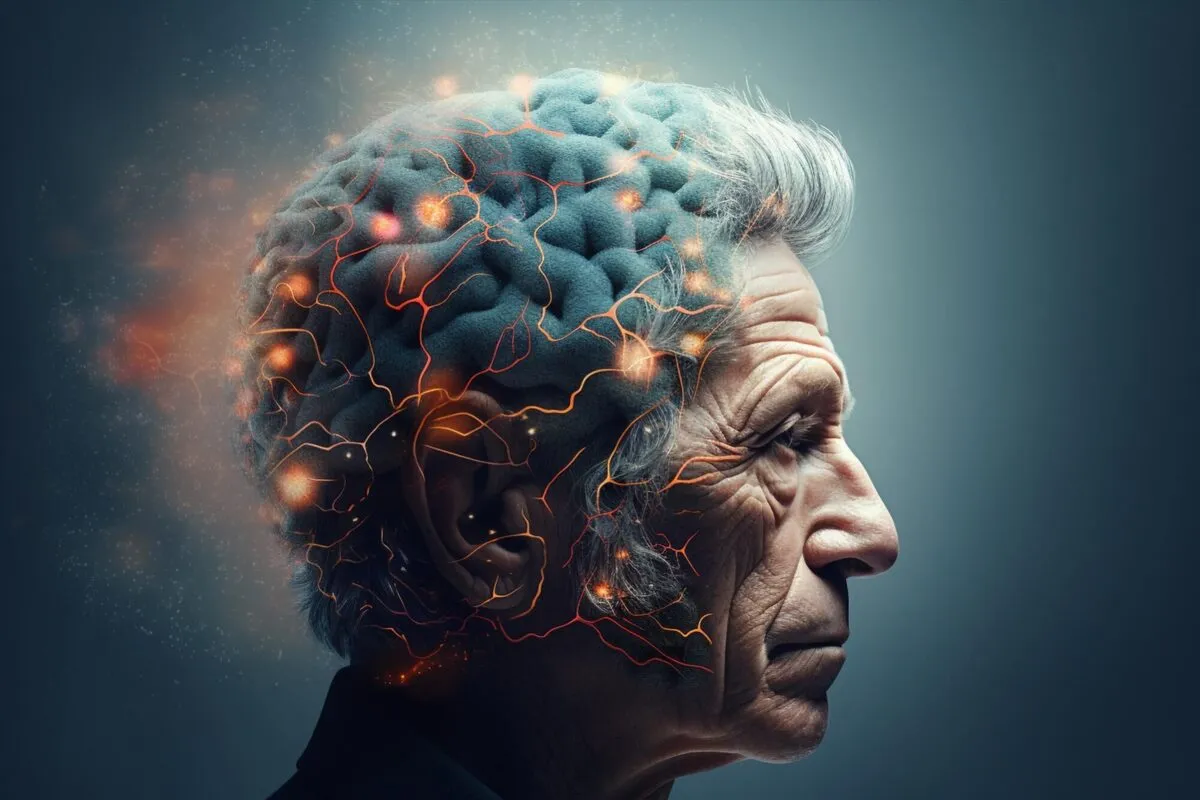
How Common Virus Could Trigger Alzheimer’s Disease
Their study suggests that the tau protein, typically seen as detrimental, might initially act as a defensive mechanism in the brain. This groundbreaking finding opens up new possibilities for treatment strategies that target both infections and the brain’s immune reactions. The findings were published in Cell Reports.
Researchers at the University of Pittsburgh have discovered a surprising connection between Alzheimer’s disease and herpes simplex virus-1 (HSV-1), suggesting that viral infections might influence the development of the condition. The study also sheds new light on tau protein, a key player in Alzheimer’s. While generally considered harmful, tau may initially help protect the brain against the virus. However, over time, it appears to contribute to brain damage. These insights could pave the way for innovative treatments that target infections and fine-tune the brain’s immune response.
“Our study challenges the conventional view of tau as solely harmful, showing that it may initially act as part of the brain’s immune defense,” said senior author Or Shemesh, Ph.D., assistant professor in the Department of Ophthalmology at Pitt. “These findings emphasize the complex interplay between infections, immune responses, and neurodegeneration, offering a fresh perspective and potential new targets for therapeutic development.”
The scientists identified forms of HSV-1-related proteins in Alzheimer’s brain samples, with greater amounts of viral proteins co-localized with tangles of phosphorylated tau – one of the hallmarks of Alzheimer’s disease pathology – in brain regions especially vulnerable to Alzheimer’s across disease stages.
Further studies on miniature models of human brains in a Petri dish suggested that HSV-1 infection could modulate levels of brain tau protein and regulate its function, a protective mechanism that seemed to decrease post-infection death of human neurons.
While the precise mechanisms by which HSV-1 influences tau protein and contributes to Alzheimer’s disease are still unknown, Shemesh and his colleagues plan to explore those questions in future research. They aim to test potential therapeutic strategies that target viral proteins or fine-tune the brain’s immune response and investigate whether similar mechanisms are involved in other neurodegenerative diseases, such as Parkinson’s disease and ALS.
4155/v





















