Scientists Discover Drug That Could Finally End Long COVID Suffering
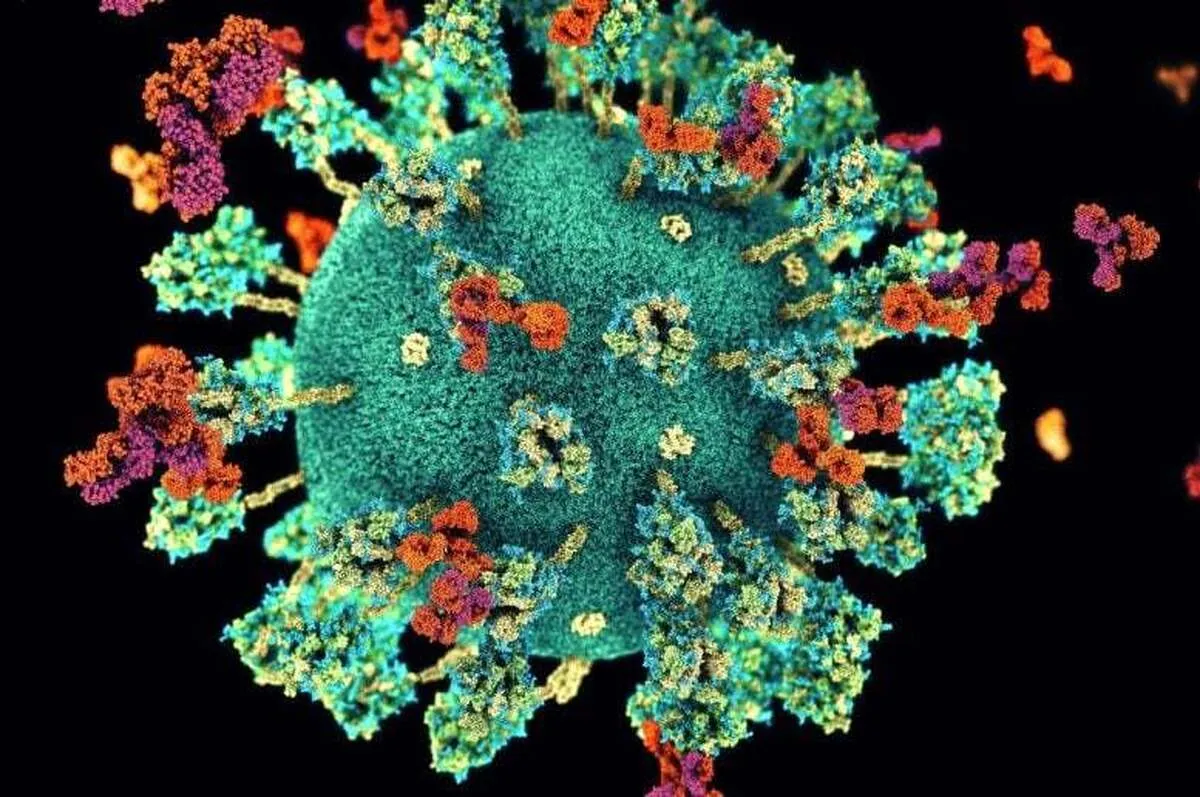
Researchers have discovered that a new drug compound can prevent long COVID symptoms in mice, a major breakthrough that could pave the way for future treatment of this debilitating condition, the journal Nature Communications reported.
In this world-first study, mice treated with the antiviral compound, developed by a multidisciplinary team at WEHI, were protected from long-term brain and lung dysfunction, two hallmark symptoms of long COVID.
The research team hopes these groundbreaking results will lead to clinical trials and eventually the first approved treatment for the condition.
Long COVID, also known as post-acute sequelae of COVID-19 (PASC), is a chronic illness marked by symptoms that persist for weeks or months after the initial infection.
It is a significant health burden that remains poorly understood – with symptoms ranging from breathing difficulties to brain fog and chronic fatigue.
Despite millions of people worldwide reporting these symptoms, the cause of long COVID remains largely unknown and there is no approved treatment for the disease.
Corresponding author and WEHI Laboratory Head, Dr Marcel Doerflinger, said the landmark results could be a turning point in the hunt for treatments to support people at risk of developing this condition.
“With 5% of people who contract COVID-19 going on to develop long COVID, the disease has morphed into a silent pandemic where millions are battling symptoms with more questions than answers,” Dr Doerflinger said.
“Our pre-clinical studies have achieved something no currently approved therapy has done to date – preventing the most debilitating symptoms of long COVID in mice.
“While more research is needed to develop a drug that can be used in humans, seeing these milestone results in the unique mouse models developed at WEHI suggests this could be a real possibility in the future, which is incredibly exciting.”
While currently approved therapies for COVID-19 like Paxlovid target a critical coronavirus protein known as Mpro, WEHI researchers identified another protein, termed PLpro, as a promising drug target in 2020.
Professor David Komander has spent over 15 years studying the family of proteins that includes PLpro and co-led the large, multidisciplinary WEHI team that spearheaded the discovery of new PLpro inhibitors.
To find a new drug compound that could target this critical protein, the team turned to the National Drug Discovery Centre (NDDC), headquartered at WEHI.
“Existing drugs had hit several hurdles to be effective in blocking PLpro in cells – our team wanted to see if we could find new ones capable of overcoming these barriers,” Prof Komander, a corresponding author and Division Head at WEHI, said.
“In order to do this, we screened over 400,000 compounds to see if we could uncover novel drug-like molecules that had potential against this protein.
“To have identified a drug target and then develop a novel drug compound against it in less than five years is an incredible feat that would have been impossible without the advanced technologies, speed and scale of the NDDC and multidisciplinary team at WEHI.”
Dr Shane Devine, a co-first and corresponding author on the paper, said the team also found their novel compound can potentially treat acute COVID better than currently available antivirals for the disease.
“Our study has provided the first evidence to prove PLpro is a powerful new drug target for COVID-19 treatments, while also showing its potential ability to treat the virus with unprecedented efficacy,” Dr Devine said.
Paxlovid is the leading COVID-19 treatment, but is currently only recommended for people who are considered at risk of severe disease.
A key limitation of this treatment is that it requires two compounds to interact with each other for the treatment to be effective – meaning it can also interfere with many other medications.
“Paxlovid and other antivirals in the market target Mpro and have these same issues, highlighting the urgent need for more research to enhance COVID-19 treatments that can provide greater access to more patients,” Dr Devine said.
“The SARS-CoV-2 virus also continues to mutate, meaning it’s only a matter of time until Paxlovid will no longer work. Our findings could lead to a future drug to help close these critical gaps.”
The project will continue collaborating with the Centre for Drug Candidate Optimisation (CDCO) and the Monash Institute of Pharmaceutical Sciences (MIPS) to evaluate the biopharmaceutical properties of this antiviral compound.
4155/v





















