Are Scientists Worried about Monkeypox Virus' Mutation?
The scientists found in one sample collected from an infected person, a large chunk of the virus’s genome was missing, and another chunk had moved to an entirely different spot in the sequence, the Nature reported.
Crystal Gigante, a microbiologist at the US Centers for Disease Control and Prevention in Atlanta, Georgia, was called in to help examine the mutations. She and her colleagues found similar deletions and rearrangements in a handful of other monkeypox genomes collected in the United States, according to a report that they posted on 17 September on the preprint server bioRxiv that has not undergone peer review.
Although scientists aren’t alarmed, they are monitoring the situation carefully to understand why the alterations have appeared, and what they might mean for the global monkeypox outbreak. These mutations are a stark reminder that even poxviruses — which are DNA viruses that tend to evolve more slowly than RNA viruses, such as the SARS-CoV-2 coronavirus — will change over time, says Elliot Lefkowitz, a computational virologist at the University of Alabama at Birmingham. And the more the monkeypox virus is transmitted between humans, he adds, the more opportunities it will have to evolve.
The mutations assessed by Gigante weren’t the single-letter alterations that scientists are used to seeing in the SARS-CoV-2 genome. In some cases, entire genes had vanished: a stretch of about 7% of the genome was missing in a sample from an infected person in Florida. But it’s too early to tell whether the mutations are beneficial, neutral or harmful to the virus, Lefkowitz says. If health officials detect an uptick in the number of virus samples carrying these mutations, that could be a possible signal that they are helping the virus to spread.
The large deletions and rearrangements that were first reported in Minnesota did not surprise Eneida Hatcher, an evolutionary virologist at the National Center for Biotechnology Information in Bethesda, Maryland. In 2015, she co-authored a study2 with Lefkowitz showing that such mutations are common in most poxviruses, and that the majority of genes that they disrupt are located towards the end, or terminal, regions of the viral genome. “It was really nice to see some of the mutational strategies replicated that we have seen in the past,” Hatcher said.
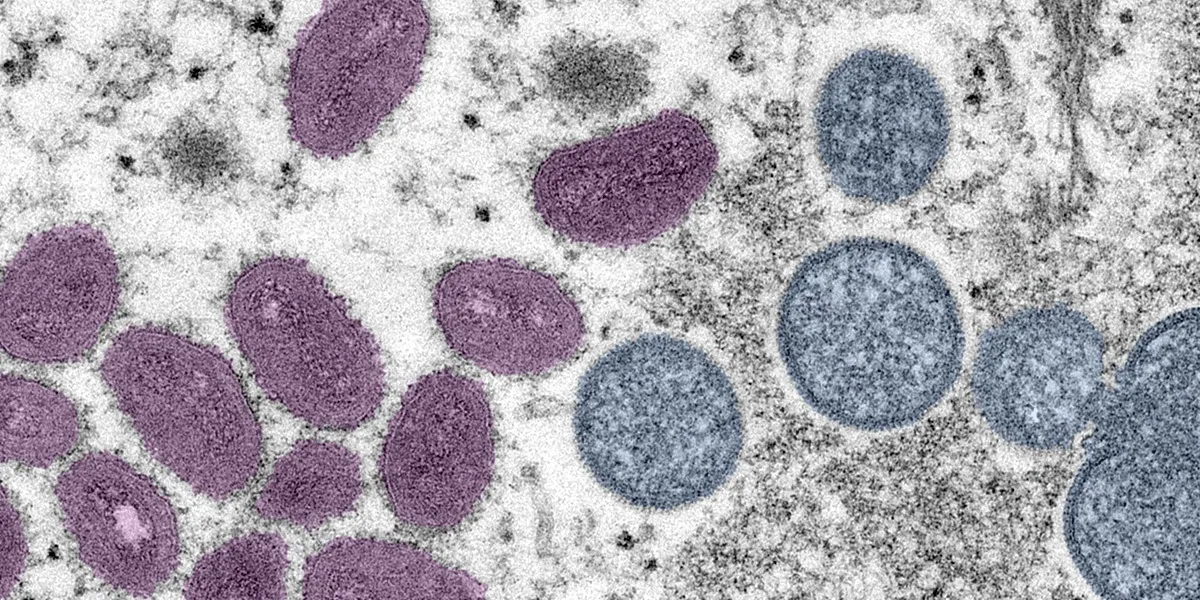
Orthopoxviruses, a genus of poxviruses that includes the monkeypox virus and the variola virus, which causes smallpox, share a core set of about 174 genes at the centre of their genomes. But their terminal regions are more variable and contain fewer essential genes. Some of the genes in these regions are thought to encode proteins that help to disarm hosts’ immune responses, and are tailored for infecting specific hosts, Lefkowitz says. This underlies one hypothesis for why variola became adept at infecting humans: over the span of thousands of years, an earlier version of the virus might have lost genes from its termini that had enabled it to infect a broad range of animal species, and it eventually became a specialist at infecting humans. (Before smallpox was eradicated, it killed about three out of ten people who were infected with it.)
Some scientists worry that a similar situation could arise with monkeypox, which is currently more of a generalist; it can infect many mammals, including several rodent species and humans.
But predicting how the monkeypox virus’s behaviour will change as it mutates is difficult because researchers have not yet characterized the function of many genes in its large genome. For example, although researchers first discovered that two strains of the monkeypox virus were spreading in Africa more than 17 years ago, they are still struggling to determine precisely which genes are responsible for the difference in death rate between the two, Lefkowitz said. The mortality rate for one of them — clade I, which is predominant in Central Africa — is about 10%. Clade II, which circulates in West Africa, has a death rate of about 1% to 3%.
By analysing monkeypox sequences, researchers are also learning more about how the virus might have sparked the global outbreak. Scientists have noticed a pattern of single-letter mutations, separate from the changes first spotted in Minnesota, that seems to be a genetic imprint of the ongoing battle between the human immune system and the virus. By using data collected so far to roughly calculate the number of these mutations expected each year, they have estimated that the strain responsible for the global outbreak jumped from animals into humans in early 2016. That’s more than a year and a half before the strain was detected in humans for the first time by Nigerian health officials, who declared an outbreak in their country that has never completely ended.
The good news is that, although the monkeypox virus continues to evolve, no mutations have affected the part of its genome that encodes a protein targeted by tecovirimat, an antiviral drug being tested for use against monkeypox in humans. But problems might eventually emerge in diagnostic testing. To detect monkeypox virus in samples, technicians perform a polymerase chain reaction (PCR) to detect target sequences in the virus’s genome. Gigante and her colleagues found that one of two copies of a monkeypox target had been deleted in one of the samples that they had analysed. Although the PCR test returned a positive result, the authors warn that these types of mutation could eventually render it ineffective.
The global attention on monkeypox will help researchers to understand not only the virus that causes the disease, but also poxviruses more generally, Hatcher says. Before this year, only about 100 near-complete monkeypox genomes existed, she says. Now, around 2,000 have been deposited into established international repositories. “I’m very happy to see the international collaborative attitude towards surveillance and genomic sequences” has continued beyond the COVID-19 pandemic, she said.
4155/v





















